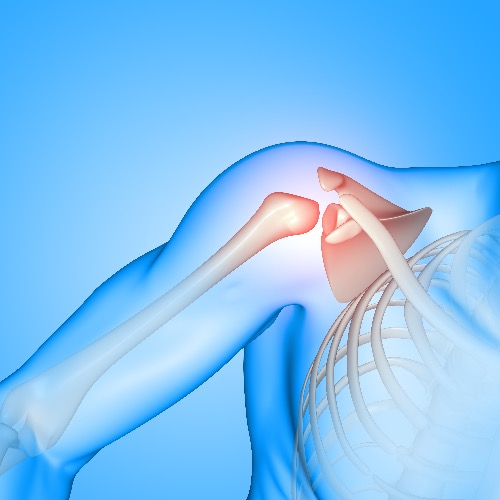
Shoulder stabilization surgery, also known as arthroscopic labral repair, is designed to repair damage to the shoulder joint and ligaments to restore stability. The shoulder joint is made up of a ball (humeral head) and a shallow socket (glenoid). The socket is lined with cartilage, known as the labrum, which helps provide stability. Soft tissues, such as muscles and ligaments, work to keep the ball firmly in place within the socket. When the shoulder rotates too far, the ligaments tighten and prevent the ball from slipping out of the socket (a dislocation).
Shoulder instability occurs when the labrum or other soft tissues are damaged, resulting in symptoms like pain, dislocation, and a sensation of looseness in the joint. Shoulder instability may manifest as single or multiple full dislocations, partial dislocations (subluxation), or persistent pain without actual dislocation. Over time, if instability is not addressed, it can gradually lead to the wear and tear of the joint, potentially resulting in arthritis, which can further complicate movement and overall joint health.
Shoulder instability arises from a Bankart injury, where the labrum and the attached ligaments are detached from the shoulder socket bone. This injury is caused by a full shoulder dislocation but can also occur when the shoulder is forcefully stretched or twisted in an abnormal direction without an actual dislocation. Dislocations are most commonly anterior (towards the front), though they can occasionally be posterior, in which case the damage occurs at the back of the socket. In some cases, only the ligaments and capsule are stretched without detaching from the labrum, which is common in people with hypermobile joints or those who are “double-jointed”.
The two primary types of surgery are: arthroscopic labral repair, which addresses minor tears in the cartilage, and Bankart repair, a more intensive procedure that reattaches and tightens the labrum and ligaments, often used when there is significant damage to the joint’s front.
Non-operative treatment for shoulder instability includes rest, physiotherapy, and avoiding activities that cause looseness or dislocations. While this approach may work, young, active individuals are more likely to experience a repeat dislocation. Early surgical intervention following the first dislocation significantly reduces the chances of future dislocations and prevents further looseness. Surgery performed early on has a much higher success rate than waiting until the shoulder has been unstable for months or years, or after multiple dislocations. The longer the instability lasts or the more dislocations that occur, the greater the chance of developing arthritis. In older or less active individuals, non-surgical methods are preferred, with surgery considered only if the instability continues.