Deluxe Accommodation Options.
Mandarin Grove and Wellbeing with 7/24 after-care facilities
Shoulder Stabilization Surgery
Treatment Process

7 Nights
Total Stay
Rigorously conducted follow-up checks
Thorough medical assessment
Regular UK consultations
Professional patient guidance
1 night stay at our partner, fully registered private hospital with English speaking chaperone attending to hospital stay for 7/24 after-care facilities.
Contact us for a Treatment Plan
Contact us for a Treatment Plan
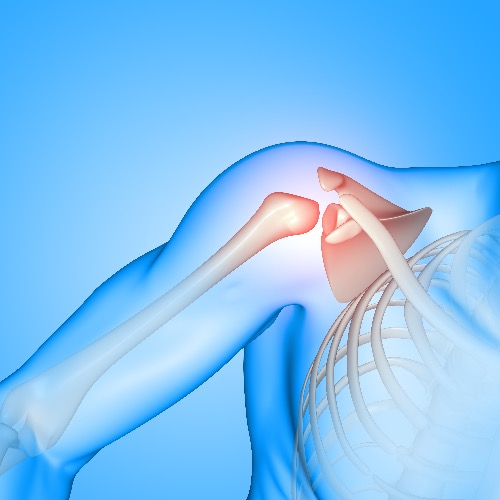
Shoulder Stabilization Surgery
Shoulder stabilization surgery, also known as arthroscopic labral repair, is designed to repair damage to the shoulder joint and ligaments to restore stability. The shoulder joint is made up of a ball (humeral head) and a shallow socket (glenoid). The socket is lined with cartilage, known as the labrum, which helps provide stability. Soft tissues, such as muscles and ligaments, work to keep the ball firmly in place within the socket. When the shoulder rotates too far, the ligaments tighten and prevent the ball from slipping out of the socket (a dislocation).
Shoulder instability occurs when the labrum or other soft tissues are damaged, resulting in symptoms like pain, dislocation, and a sensation of looseness in the joint. Shoulder instability may manifest as single or multiple full dislocations, partial dislocations (subluxation), or persistent pain without actual dislocation. Over time, if instability is not addressed, it can gradually lead to the wear and tear of the joint, potentially resulting in arthritis, which can further complicate movement and overall joint health.
Shoulder instability arises from a Bankart injury, where the labrum and the attached ligaments are detached from the shoulder socket bone. This injury is caused by a full shoulder dislocation but can also occur when the shoulder is forcefully stretched or twisted in an abnormal direction without an actual dislocation. Dislocations are most commonly anterior (towards the front), though they can occasionally be posterior, in which case the damage occurs at the back of the socket. In some cases, only the ligaments and capsule are stretched without detaching from the labrum, which is common in people with hypermobile joints or those who are “double-jointed”.
The two primary types of surgery are: arthroscopic labral repair, which addresses minor tears in the cartilage, and Bankart repair, a more intensive procedure that reattaches and tightens the labrum and ligaments, often used when there is significant damage to the joint’s front.
Non-operative treatment for shoulder instability includes rest, physiotherapy, and avoiding activities that cause looseness or dislocations. While this approach may work, young, active individuals are more likely to experience a repeat dislocation. Early surgical intervention following the first dislocation significantly reduces the chances of future dislocations and prevents further looseness. Surgery performed early on has a much higher success rate than waiting until the shoulder has been unstable for months or years, or after multiple dislocations. The longer the instability lasts or the more dislocations that occur, the greater the chance of developing arthritis. In older or less active individuals, non-surgical methods are preferred, with surgery considered only if the instability continues.
Who are the eligible candidates for shoulder stabilisation surgery?
Shoulder stabilization surgery is often recommended for individuals with recurrent shoulder dislocations or those at high risk of dislocating again, such as athletes in contact sports. When nonsurgical options such as physical therapy and rest have not alleviated the issue, surgery becomes a viable solution to prevent further dislocations and restore function. Candidates may have experienced shoulder damage from a fall onto an outstretched arm, heavy lifting, or a sudden, forceful overhead movement.
How is shoulder stabilisation surgery performed?
Shoulder stabilization surgery is performed under general anaesthesia, although the type of anaesthesia can vary depending on the patient’s needs. The procedure typically lasts between 45 minutes and 2 hours.
The surgeon makes three or four small incisions around the shoulder and upper arm to gain access to the joint. Through these incisions, surgical instruments and a small camera (arthroscope) are inserted to allow the surgeon to view inside of the shoulder and repair the torn labrum and ligaments, removing scar tissue and repositioning damaged tissue as needed.
Recovery Facts with Shoulder Stabilisation Surgery
• Mild range of pain could be experienced but not in extreme levels though, usually well-controlled by tablets. A stronger painkiller injection may be needed occasionally. Pain should ease within a few days, but avoid overusing the shoulder too early. Avoid elevating the arm above shoulder height or rotating it excessively outward.
• The shoulder will be swollen for about 24 hours due to the sterile fluid used during surgery for better visibility of the joint.
• The dressing used during the surgery will be removed, and any soiled waterproof dressings will be replaced. These small dressings should stay in place until your two-week post-operative review.
Post-operative key points with shoulder stabilisation surgery
- A physiotherapist will guide you on exercises and the management of the sling. Use the sling for 6 weeks unless otherwise instructed.
- You are allowed to shower but avoid directly soaking the dressings.
- The sling should be worn during the day while walking around, removed during exercises and showering, and not necessary when seated or at night.
- The small wounds will usually heal well, with only faint scarring over time.
- Short-term muscle loss around the shoulder due to lack of use will occur but will return after rehabilitation over several months.
- Avoid running during this time and refrain from driving while using the sling. Exercise bike use is allowed almost immediately.
- At Prospero medical, we continue to track our patients’ recovery for 6 months up to a year after surgery, regardless of their location. Patients must report any issues directly to our clinic before consulting other specialists.
Benefits of having shoulder stabilisation surgery in Turkey
Turkey is renowned for its exceptional healthcare system and growing popularity as a medical tourism hub. Turkey seamlessly blends advanced healthcare with its captivating culture and hospitality, ensuring both your physical recovery and emotional well-being are well taken care of. If you’re considering a shoulder stabilization surgery, here are some benefits that should make Turkey stand at the top of your list:
• Highly qualified surgeons with extensive experience and a tradition of medical excellence.
• State-of-the-art hospitals equipped with the latest surgical and diagnostic technology.
• Tailored aftercare services infused with the welcoming nature of Turkish hospitality.
• Affordable treatment costs that provide great value for money without compromising quality.
• A peaceful recovery setting, often combined with rehabilitation programs including physical therapy to speed up the recovery process and opportunities to explore Turkey’s scenic beauty.
Cost implications of shoulder stabilisation surgery?
When selecting the right clinic for your surgery, it’s essential to focus on several key factors. With the overwhelming number of commercial ads and social media sales pitches, it can be a challenge identifying a clinic that meets all the necessary criteria. What should be your guiding principle as you go through the process of shortlisting the best clinic for your needs? The key criteria for choosing a clinic include:
- Providing medical advice that is honest and not influenced by commercial interests, so patients receive clear and unbiased guidance.
- Establishing a good rapport with the patient to better understand their concerns and manage their expectations.
- Placing the utmost importance on the patient’s safety and well-being, ensuring every aspect of care prioritizes their long-term health.
Determining a realistic price for treatment involves evaluating several keys factors, such as:
- The clinic’s professional reputation.
- The nature and complexity of the surgery.
- The qualifications and experience of the surgeon.
- The quality of the aftercare services.
- Clear, unbiased terms and conditions that outline clinical liabilities in a legally sound manner ensuring that both the clinic and the patient are well protected and fully aware of their rights and responsibilities throughout the process.
The cost of shoulder stabilization surgery in Turkey can vary based on the factors mentioned above. While cost may be a significant factor when considering surgery abroad, prioritizing price over quality without confirming if the clinic meets the essential criteria can lead to problems that are not only difficult to fix but also financially draining over time. At Prospero medical, we strive for transparency in our pricing. Every service component is laid out clearly, so patients are empowered to make informed decisions about their treatment. We aim to provide pricing that reflects the high level of medical care, the expertise of our surgeons, and the quality of aftercare, all backed by years of experience in the industry. Ultimately, we are dedicated to offering exceptional, high-quality care that aligns with a realistic and fair price, ensuring the best possible outcomes for our patients.